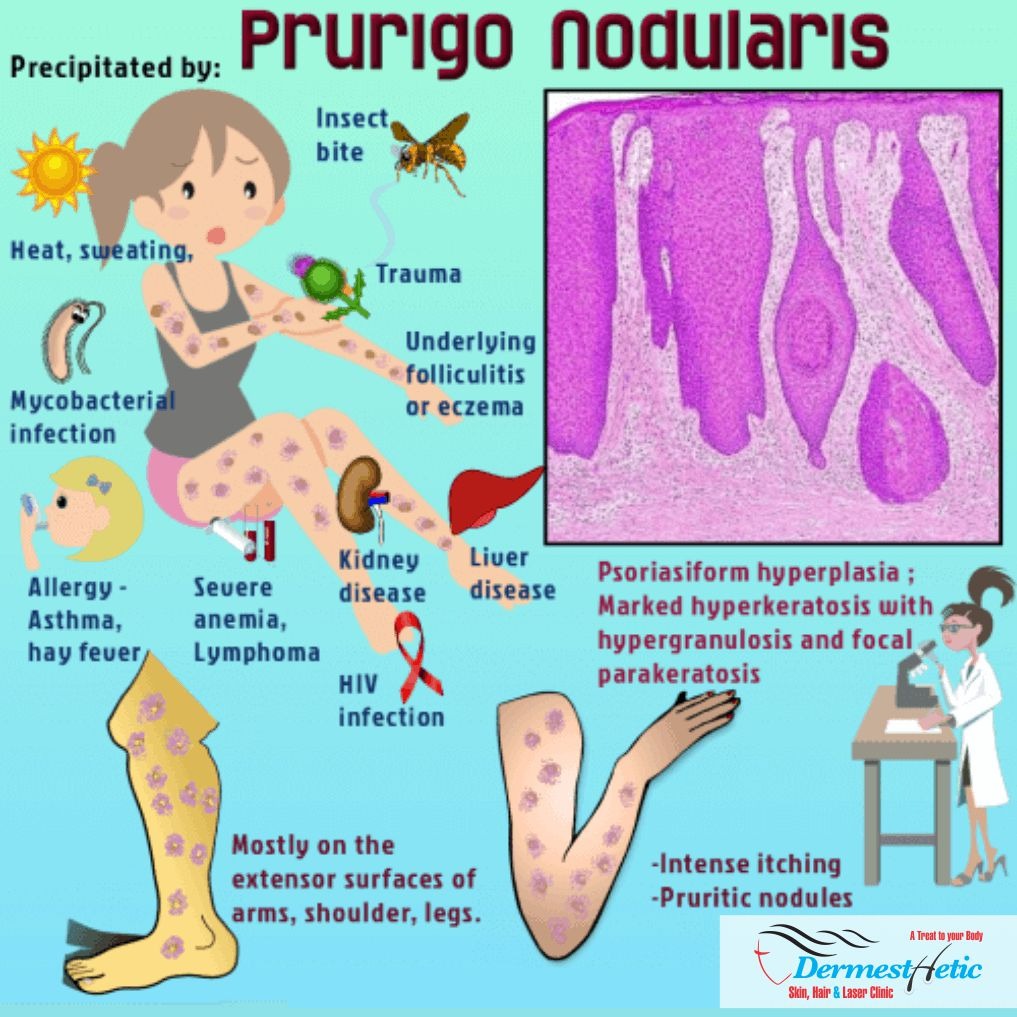
Nodular prurigo (NP) or prurigo nodularis is a chronic skin condition characterized by very itchy firm lumps. It can appear anywhere on the body but is most common on the arms, legs, back, and torso, in a symmetrical distribution. It is the most severe form of prurigo and thus can be difficult to treat. Prurigo nodularis is a chronic skin disorder characterized by the presence of hard, extremely itchy bumps known as nodules. Though the cause of the condition is unknown, the nodules are the result of persistent, intense scratching and rubbing of the skin. Doctors believe prurigo nodularis comes from a problem with your immune system and the nerves in your skin that cause you to feel itchiness more than normal. Many people who get it are already dealing with a health condition that causes itchy skin. Most often, it’s a skin problem such as Atopic dermatitis (eczema).
Prurigo nodularis is a skin condition that causes itchy bumps on your skin. It usually occurs with other skin conditions like eczema or psoriasis, but not always. The most common first-line treatments include anti-itch creams and corticosteroid injections. If you want to treat Prurigo nodularis, you should visit a dermatologist. We at DERMESTHETIC at Sialkot & Lahore, Pakistan have experienced dermatologists and skin experts diagnosing and curing these diseases.

CONSULTATION
Prurigo nodularis (PN) is a skin condition that causes hard, raised bumps on your skin. The bumps are often dry and crusty on top. They’re extremely itchy, especially at night. You might only have a few bumps or a large collection of bumps in one area. Scratching the bumps can lead to bleeding or scarring.
Prurigo nodularis can develop anywhere on your body, but it’s often on your:
- Abdomen
- Arms
- Legs
- Scalp
- Shoulders
- Upper Back
Nodular prurigo can affect both sexes and people of all ages but is more common in older adults.
There is also an association with:
- Atopy (predisposition to asthma, atopic dermatitis, and hayfever)
- Drugs that produce chronic itch such as antimalarials, opioids, and targeted cancer treatments
- HIV/AIDS
- Thyroid disorders.
- Internal disease such as:
- Chronic kidney disease
- Cancer
- Diabetes
- Liver disease
Sometimes, prurigo goes away on its own, but it’s a chronic skin condition that can last for several months or longer. The skin rash may clear up for a while and then come back. Identifying what triggers your flare-ups may help you avoid them in the future. Complications from PN are rare, but open lesions can get infected. Healed lesions may leave scars or cause skin discoloration. We at DERMESTHETIC at Sialkot & Lahore, Pakistan have such expertise and knowledge to treat amicably prurigo nodularis.
CAUSES
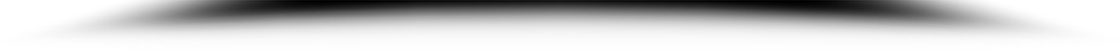
The exact cause of prurigo nodularis remains unknown. It is thought to relate to a dysregulation of the nerves as skin biopsies have shown a greater number of nerve cells in the dermis but a reduced amount in the epidermis. There is also an increased number of Merkel cells in the epidermis and the papillary layer of the dermis, as well as more neutrophils and mast cells, thus more cytokine release; which may explain the severe itchiness.
The itchiness may start as a result of an insect bite, stress, dermatitis, or another underlying skin or systemic condition. There is also an association with brachioradial pruritus, which results from traction of spinal nerves in the neck. Scratching will thicken and inflame skin, worsening the condition. Prurigo nodularis isn’t contagious. It may result from too many nerve or immune cells in your skin. Other conditions may increase itchiness on your skin’s surface, so the bumps might appear from excessive scratching and irritation. Sometimes, medication, like certain types of chemotherapy causes prurigo nodularis.

NODULAR PRURIGO (NP) SYMPTOMS
We at DERMESTHETIC at Sialkot, Lahore, Pakistan have experienced dermatologists treating the prurigo nodularis along with counselling on psychological issue which may crop up due to dermatitis/eczema and properly advise the patients regarding the treatment. Prurigo nodularis is a chronic disorder of the skin that is classically seen as multiple, firm, flesh to pink colored papules, plaques and nodules commonly located on the extensor surfaces of the extremities. The lesions are very pruritic and can occur in any age group. It is commonly associated with another disease such as atopic dermatitis or any dermatoses associated with chronic pruritus. The diagnosis is chiefly clinical. However, lichen simplex chronicus and hypertophic lichen planus may be clinically indistinguishable in many cases. Thus diagnostic confirmation with dermoscopy and histopathology becomes important. The therapeutic approach is wide-arrayed ranging from treatments that act as – potent antipruritics, immunomodulators, and neuromodulators. Treatment in an established case is prolonged and improving patient compliance with education and counseling is important.
Prurigo nodularis can be difficult to treat, taking months or even years to clear and may not resolve completely, often rendering it a chronic condition. It is important that patients follow their dermatologist’s recommendations and report any issues with the treatment so that different approaches can be used. This activity reviews the evaluation and management of prurigo nodularis, and highlights the role of the interprofessional team in caring for patients with this condition.

Objectives:
- Identify the etiology of prurigo nodularis.
- Describe the evaluation of prurigo nodularis.
- List the treatment and management options available for prurigo nodularis.
- Employ interprofessional team strategies to improve care coordination and care delivery for patients with prurigo nodularis.
TREATMENT
We at DERMESTHETIC at Silakot & Lahore, Pakistan have experienced dermatologists and therapists treating the prurigo nodularis and properly advise the patient regarding the treatment after making diagnosis. Itch relief medication (apply to your skin): Your dermatologist may recommend applying menthol, phenol, pramoxine, or capsaicin cream to help relieve the itch. These are available without a prescription. If you need a stronger medication, your dermatologist may prescribe calcipotriol or another medication.

The exact etiology of prurigo nodularis remains poorly understood. Although the role of unimpeded itch-scratch cycle is uncontested, the exact sequence of events leading to the final clinical picture remain conjectural. Prurigo nodularis is accompanied by long-standing pruritus and thought to develop as a reaction to repeated scratching in patients with chronic prurigo of various etiologies including dermatological, systemic, infectious, and neuropsychiatric.
Management of prurigo nodularis requires a multifaceted approach. Patients need to be educated on practices to reduce scratching of lesions, assurance and diagnosing of underlying causes of pruritus and diagnosis and treatment of any psychological disorder associated with scratching and picking at skin. Treatments, both topical and systemic, are targeted at disrupting the itch-scratch cycle.
GENERAL CARE
- Patients are encouraged to keep their nails short, wear protective clothing such as long sleeves and gloves, and to keep the nodules covered with bandages.
- Using gentle cleansers to bathe and applying emollients/moisturizers etc. multiple times a day to keep skin moisturized should be encouraged.
- Calamine lotions and lotions containing menthol and camphor can provide relief from the pruritus.
- Stay in a cool comfortable environment.
- Reduce stress.
The most common treatments for mild prurigo nodularis include:
Injections: You may receive an injection of medication directly into the skin lesions. Injections of corticosteroids (anti-inflammatory drugs) reduce inflammation and can help relieve pain, redness and itching right away.
Topical Treatments: You apply certain medications directly to your skin as creams or ointments. Calamine lotion is a common antihistamine (anti-itch medication). Your provider may also recommend topical corticosteroids, vitamin D or calcineurin inhibitors (immune system suppressants).
If injections or topical treatments aren’t effective, your provider may recommend:
Cryotherapy: Cryotherapy uses liquid nitrogen to freeze off large or especially itchy skin lesions. Most people receive cryotherapy in combination with corticosteroid injections.
Immunosuppressants: Immunosuppressants are drugs that prevent your immune system from overacting. You might receive this treatment if you have PN related to an autoimmune disorder, such as lupus or psoriasis.
Phototherapy: Phototherapy uses ultraviolet (UV) light to reduce itchiness and help skin lesions heal. It works by calming immune cells that release histamines. Most people need several treatments.

PREVENTIVE MEASURES
There’s no way to prevent prurigo nodularis, but you can take steps to reduce itchiness, irritation and new PN flare-ups:
- Avoid the sun or wear sunscreen with an SPF (sun protection factor) of at least 30.
- Keep your fingernails trimmed short.
- Stay out of hot environments and avoid activities that may cause sweating.
- Use gentle cleansers and moisturizers on your skin.
- Wear long sleeves and gloves.
If skin lesions break open or bleed, be sure to apply antibiotic ointment and cover the lesions with clean bandages.
SIDE EFFECTS
Side effects of PN treatments vary depending on the method you choose and the potency of the medication. Immunosuppressants can cause significant side effects and some require regular blood tests. The potential side effects for oral corticosteroids can be more serious if use continuously. Antibiotics can give you an upset stomach or make you dizzy and lightheaded. Overexposure to ultraviolet light during phototherapy carries its own risks, particularly that of skin cancer. Discussion with the patient should include advantages and disadvantages of the therapy, side effects and possible use of off-label medications. Patient education can thus promote treatment adherence. The potential length of therapy should also be discussed as prurigo nodularis is difficult to treat and the patient may become frustrated with lack of improvement.
Lesions of prurigo nodularis can become secondarily infected due to scratching of the lesions. It is important to monitor for clinical signs of infection such as erythema, pain, warmth and fever. If secondary infection is suspected, it is important to begin appropriate topical or systemic antibiotic therapy to cover for skin flora. The deterrents in prurigo nodularis treatment are the severe intensity of the itch which can lead to psychological distress, chronic nature of the condition, the long duration of the therapy and the potential side effects of the medication.

DR. BUSHRA BASHIR
M.B;B.S, FCPS (DERMATOLOGY)
FELLOWSHIP DIPLOMA IN FACIAL AESTHETIC (USA)
ASSISTANT PROFESSOR (AIMC)
STEM CELLS EXPERT
MEMBER AMERICAN BOARD OF REGENERATIVE MEDICINE
CONSULTANT DERMATOLOGIST & COSMETOLOGIST
Skin, Hair & Laser Specialist
Cell: 00 92 332 444 7284, 042-353 40228
contact@dermesthetic-clinic.com
54 Commercial, Ground Floor, Umer Block, Sector-B
Near Bahria Town Safari Villa Zoo, Bahria Town, Lahore.